- The case demonstrates that older adults with blood cancers who receive reduced intensity chemotherapy before a stem cell transplant with donor cells that are resistant to HIV may be cured of HIV infection
- City of Hope’s expertise treating older blood cancer patients with reduced intensity chemotherapy and HIV patients with cancer helped the patient achieve remission for both diseases
City of Hope®, one of the largest cancer research and treatment organizations in the United States, treated the oldest person to be cured of a blood cancer and then achieve remission for HIV after receiving a blood stem cell transplant from a donor with a rare genetic mutation. Research published in NEJM today demonstrates that older adults with blood cancers who receive reduced intensity chemotherapy before a stem cell transplant with donor cells that are resistant to HIV may be cured of HIV infection.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20240214747351/en/
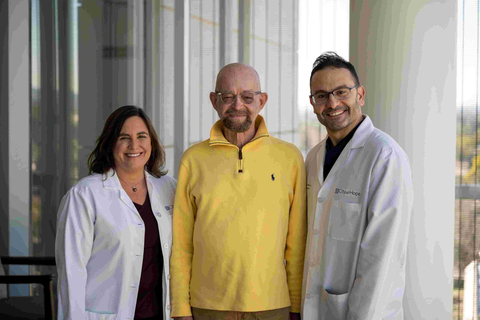
"City of Hope Patient" Paul Edmonds with City of Hope doctors, Jana K. Dickter, M.D., and Monzr Al Malki, M.D. (Photo: Business Wire)
Paul Edmonds, 68, of Desert Springs, California, is the fifth person in the world to achieve remission for acute myelogenous leukemia and HIV after receiving stem cells with a rare genetic mutation, homozygous CCR5 Delta 32. That mutation makes people who have it resistant to acquiring HIV. Edmonds is also the person who had HIV the longest — for over 31 years — among these five patients.
Known as the “City of Hope patient” among these five patients, Edmonds received a transplant at City of Hope on Feb. 6, 2019, and is now considered to be cured of leukemia. Edmonds stopped taking antiretroviral therapies for HIV nearly three years ago and will be considered cured of HIV after he has stopped taking antiretrovirals for five years. Read Edmonds’ story here and view a video here.
“City of Hope’s case demonstrates that it is possible to achieve remission from HIV even at an older age and after living with HIV for many years,” said Jana K. Dickter, M.D., a clinical professor in City of Hope’s Division of Infectious Diseases, who led the study. “Furthermore, remission can be achieved with a lower-intensity regimen than the therapy received by the four other patients who went into remission for HIV and cancer. As people with HIV continue to live longer, there will be more opportunities for personalized treatments for their blood cancers.”
For Edmonds’ medical team, this meant they would need to tailor his treatment to address his age and the duration of his HIV. City of Hope’s decades-long expertise treating older adults with cancer and HIV — efforts led by John A. Zaia, M.D., director of City of Hope’s Center for Gene Therapy and Aaron D. Miller and Edith Miller Chair for Gene Therapy, and other doctors — proved to be invaluable in treating Edmonds and helping him go into remission for both leukemia and HIV.
Under the care of City of Hope hematologist Ahmed Aribi, M.D., assistant professor in the Division of Leukemia and a study author, Edmonds received three different therapies to get him into remission before receiving a transplant. The therapy is needed to help the patient achieve remission, and the patient can then proceed with a transplant with the goal of curing the cancer.
Edmonds received a chemotherapy-based, reduced-intensity transplant regimen prior to his transplant that was developed by City of Hope and other transplant programs for treatment of older patients with blood cancers. Reduced-intensity chemotherapy makes the transplant more tolerable for older patients and reduces the potential for transplant-related complications from the procedure.
For the transplant, Aribi and his team worked with City of Hope’s Unrelated Donor Bone Marrow Transplant Program — directed by Monzr M. Al Malki, M.D. — to find a donor who was a perfect match for the patient and had the rare genetic mutation, which is found in just 1-2% of the general population.
The mutation makes people who have it resistant to acquiring HIV. CCR5 is a receptor on CD4+ immune cells, and HIV uses that receptor to enter and attack the immune system. But the CCR5 mutation blocks that pathway, which stops HIV from replicating.
Edmonds had mild to moderate side effects caused by graft-versus-host disease, which occurs when the donor’s T lymphocytes, a type of white blood cell that fights infections, attack the patient’s cells.
Edmonds also achieved “full chimerism,” meaning that all of his bone marrow and blood stem cells originated from the donor.
Stephen J. Forman, M.D., director of City of Hope’s Hematologic Malignancies Research Institute and a professor in the Department of Hematology & Hematopoietic Cell Transplantation, noted a confluence of several research initiatives by City of Hope over the years helped lead the institution to this moment.
“City of Hope and other institutions started performing successful stem cell transplants in older adults a decade ago, an intensive and high-risk procedure in this population that was unheard of prior to then,” Forman said. “We have treated patients who are in their 80s with transplants and that is due to City of Hope’s emphasis on expanding therapies to more patients, as well as our compassionate, top-notch care of even the most vulnerable populations.
“City of Hope is not stopping there. Our researchers are working on creating stem cells that have the genetic mutation that makes them naturally resistant to HIV, among other research initiatives,” he added.
These milestones include:
- City of Hope was one of the first institutions in the United States to perform a reduced intensity regimen for older patients with myelodysplasia, a blood disease that can evolve into leukemia and that Edmonds had prior to acute myelogenous leukemia.
- Ryotaro Nakamura, M.D., director of City of Hope’s Center for Stem Cell Transplantation and Jan & Mace Siegel Professor in Hematology & Hematopoietic Cell Transplantation, led the national trial that demonstrated a transplant could become standard of care for older people with myelodysplastic syndromes, which led to Medicare approving the therapy in older populations.
- City of Hope was one of the first centers in the United States to perform effective, curative autologous transplants, which use a person’s own stem cells, for patients with HIV-related lymphoma. When many centers still treated patients with low-intensity, noncurative treatment approaches, City of Hope — led by Forman and Amrita Krishnan, M.D., executive medical director of hematology, City of Hope Orange County – challenged that paradigm by demonstrating that autologous transplants could be used to cure patients with HIV-related lymphomas who would otherwise die.
- City of Hope was also a primary national co-leader in two National Cancer Institute-sponsored trials for autologous as well as allogeneic stem cell transplantation, which use a donor’s stem cells, for patients with HIV and blood cancers. Led by Joseph Alvarnas, M.D., City of Hope’s vice president of government affairs and a hematology professor, these trials led to a change in the national standards of care on how best to manage this vulnerable patient population.
City of Hope’s blood stem cell and bone marrow transplant (BMT) program has performed nearly 19,000 transplants, making it one of the largest programs in the nation. City of Hope has exceptional transplant outcomes year after year, according to the Center for International Blood & Marrow Transplant Research.
Building on its BMT expertise, City of Hope is also a pioneer in the development of chimeric antigen receptor (CAR) T cells to treat blood cancers and solid tumors. More than 1,200 patients have been treated with CAR T cell therapy at City of Hope.
Leveraging their expertise in cellular immunotherapy, City of Hope scientists have also developed chimeric antigen receptor CAR T cells that can target and kill HIV-infected cells and control HIV in preclinical research. A City of Hope clinical trial using CAR T cell therapy, which has the potential to provide HIV patients with a lifelong viral suppression without antiretroviral therapies, is expected to open later this year.
Angelo Cardoso, M.D., Ph.D., City of Hope director of the Laboratory of Cellular Medicine, is also a study author and performed many of the experiments that confirmed Edmonds’ HIV remission.
About City of Hope
City of Hope's mission is to make hope a reality for all touched by cancer and diabetes. Founded in 1913, City of Hope has grown into one of the largest cancer research and treatment organizations in the U.S. and one of the leading research centers for diabetes and other life-threatening illnesses. City of Hope research has been the basis for numerous breakthrough cancer medicines, as well as human synthetic insulin and monoclonal antibodies. With an independent, National Cancer Institute-designated comprehensive cancer center at its core, City of Hope brings a uniquely integrated model to patients spanning cancer care, research and development, academics and training, and innovation initiatives. City of Hope’s growing national system includes its Los Angeles campus, a network of clinical care locations across Southern California, a new cancer center in Orange County, California, and treatment facilities in Atlanta, Chicago and Phoenix. City of Hope’s affiliated group of organizations includes Translational Genomics Research Institute and AccessHope™. For more information about City of Hope, follow us on Facebook, X, YouTube, Instagram and LinkedIn.
View source version on businesswire.com: https://www.businesswire.com/news/home/20240214747351/en/
Contacts
Letisia Marquez
626-476-7593
lemarquez@coh.org